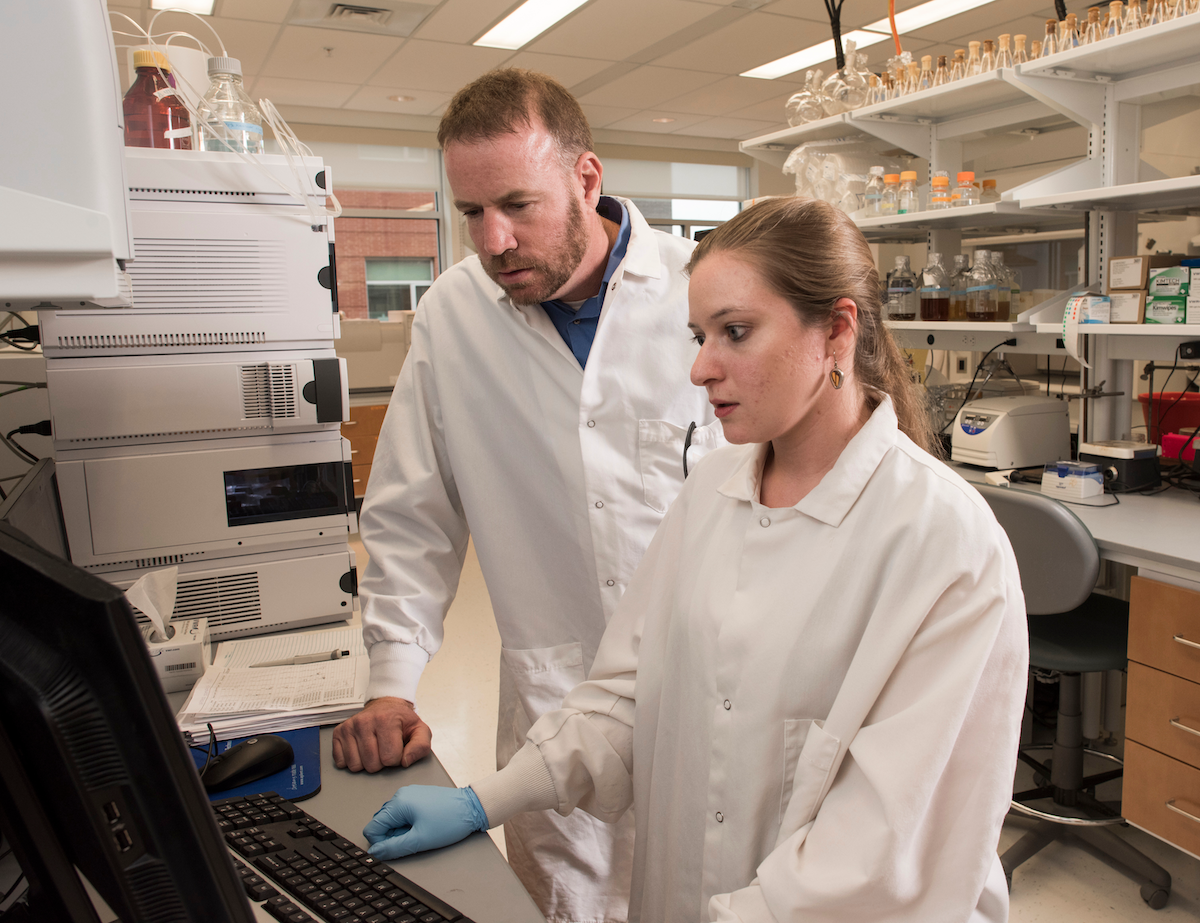
With COVID-19 continuing to spread throughout the world, there is a demand for rapid, noninvasive diagnostics. George Mason University researchers Robin Couch and Allyson Dailey, members of the College of Science and the Institute of Biohealth Innovation, are working to answer that call with their research on volatile organic compounds (VOCs) for infectious disease detection.
VOCs are gases that emanate from a variety of sources, including from humans. Much like a sommelier can smell wine and determine the composition of it, Couch and Dailey have been looking at the scent prints of bacteria. They have been able to successfully diagnose mice infected with biothreat agents using this method, and were able to differentiate standard bacteria strains from antibiotic-resistant strains, as seen in Nature Scientific Reports. Mason holds a patent around the technology on the extraction and analysis of gases through the VOC extraction chamber.
When the news of COVID struck the world in March 2020, the researchers embraced it as an opportunity to further test their approach on viruses. Through a partnership with Sentara Healthcare, trained nurses collected breath samples to support Couch and Dailey’s study, as well as performed the test for standard patient care. The research team analyzed the breath samples, compared results from the traditional diagnostic test, and trained their instrument on the difference in VOCs between positive and negative COVID results. From there, they were able to take the breath samples and quickly discern whether or not a patient had COVID-19.

“Sentara Northern Virginia Medical Center is excited to collaborate with George Mason University on this cutting-edge research,” said Heather Causseaux, director of patient care services. “We hope this study not only leads to advancements in patient care, but also the health care industry.”
The idea to use VOCs for COVID-19 diagnostics originated from a study in collaboration with Mason Science Associate Dean for Research Pat Gillevet and Rush University. The team looked at the scent profile of fecal samples from healthy patients and from those who were clinically diagnosed with alcoholism to assist with detecting the disease. Couch and Dailey’s goal then shifted toward using the technique for diagnostics.
Not only is VOC analysis less invasive than conventional diagnostic testing using biofluids, such as urine, but it also has broad applicability in the medical field. Rather than needing a battery of tests, VOC analysis can simultaneously look for multiple diseases using the same sample and technique. In fact, the researchers are optimistic that one day, scent analysis can be used for early disease intervention during regular checkups.
“Imagine being able to receive a whole body analysis through your scent profile when you go to your general practitioner,“ said Couch. “An instrument would be able to compare your scent to a library of diseases and promptly determine whether or not you have indicators of illnesses like diabetes or Parkinson’s disease, meaning you’re able to receive treatment sooner, or prevent the illness entirely.”
Another direction where the team would like to eventually take their VOC analysis testing capabilities is a surveillance tool. For instance, Couch and Dailey envision that as individuals walk by a testing station, it could smell their VOCs and provide rapid diagnostic information in the form of green, yellow, and red lights based on the detection of transmissible diseases. This could be especially valuable in public settings like schools and airports.
The researchers use the technique’s potential to help others as motivation for continuing to pursue their studies.
“What excites me most about our investigation is knowing what I’m working on right now could be used to help a lot of people,” said Dailey. “That’s what keeps me moving forward.”
